NVIDIA: How Deep Learning Can Determine Drug Treatments for Better Patient Outcomes
OREANDA-NEWS. May 18, 2016. The stakes could hardly be higher in pediatric intensive care units.
Children arrive with complex, often chronic conditions, including respiratory illnesses, trauma, post-surgical care issues, sepsis and other infections. Many come as emergency cases.
To find the best drug treatments for them, David Ledbetter, a data scientist at the Children’s Hospital Los Angeles, and his team of researchers, are using GPU-powered deep learning to digest big data — a decade’s worth of health records from the pediatric ICU.
Ledbetter has a simple primary goal: optimizing patient outcomes.
“When you look in a pediatric ICU room, what you see are millions of wires,” he said in a packed talk at the recent GPU Technology Conference in Silicon Valley.
“What you can’t often see is that there’s a patient there, too. We want the focus on the patient,” he said.
Harnessing Big Data
Increasingly powerful GPUs allow scientists to apply deep learning, a fast-developing branch of artificial intelligence, to teach computers to learn to see patterns in giant datasets.
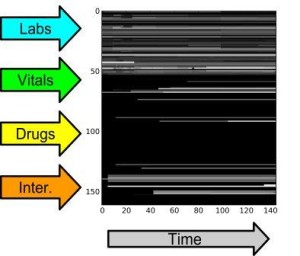
To train its deep learning models, Ledbetter’s team created nearly 13,000 so-called “patient snapshots” from the records of patients who passed through the pediatric ICU at Children’s Hospital Los Angeles.
The snapshots detail interactions between a patient’s vital state, heart rate, blood pressure and the treatments they were given. Ledbetter and his team fed these into two separate neural network models, using TITAN X GPUs to complete the training in a matter of hours.
Improving Outcomes
With a convolutional neural network, they were able to predict the probability of survival, and with a recurrent neural network, they could predict physiology through time. This aided their understanding of the key relationships between the patient’s vitals and the interventions performed in the unit.
“The hope was that if you can get a patient into a stable state, then the patient’s own defenses will take over,” Ledbetter said.
“Doctors are focused on survival over time, and there’s a big difference with an 80 percent chance of survival, which during the course of an hour drops to 50 percent, so we measure treatments in terms of changing the outcome.”
In the critical time available to make life-saving decisions, “we can make an impact,” Ledbetter said. Putting the information into the hands of doctors, helps “make sure we’re doing everything in our power to use the information to treat kids better.”




Комментарии